Definition of Medical Ethics
Miscellanea / / July 04, 2021
By Florencia Ucha, in Dec. 2012
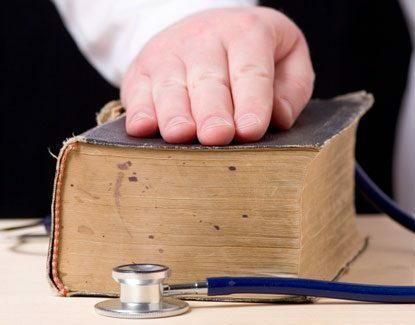 The ethics Medical is that branch of ethics that is concerned with promoting the ethical principles that regulate the activity of medicine so that a correct action by health professionals always prevails in relation to the patients they treat.
The ethics Medical is that branch of ethics that is concerned with promoting the ethical principles that regulate the activity of medicine so that a correct action by health professionals always prevails in relation to the patients they treat.
Branch of ethics that promotes principles and values among medical professionals: respect and conscience in the treatment of patients
In other words, it should shed light on what should and should not be done in specific cases.
The importance of this branch of ethics arises especially from the need to regulate medical activity in a context such as that of our days in which technological advances and scientific discoveries are running, and therefore open new possibilities of Act.
That is, this scenario has brought the possibility of treating a disease from several proposals, but of course, using them does not always apply, and it is at this point where medical ethics must intervene to order the situation and guarantee the patient that he will be treated with I respect Y conscience.
Medical ethics will judge medical acts based on four essential principles: beneficence, non-maleficence, justice and autonomy, and Thus it is that the actions of physicians and of all the actors that intervene in the context of health must be guided by the themselves.
The ethics is a discipline that takes care of study of the moraland from that approach it will tell us which is the behavior that is expected of the people who make up this or that society.
It should be noted that the moral It is a concept that goes hand in hand with that of ethics and that involves the set of actions and behaviors regulated and typified in good and bad, and that will guide the behaviors of the society in which they are imposed.
Basically, what ethics does is establish which are the most valuable and respectable behaviors and behaviors and which are located on the totally opposite side.
Then, once they are identified, they will be regulated and thus will be established and socially agreed on what is good, bad, fair, unfair, among others and ultimately, what is ethically desirable and what is not it is.
Ethics, for example, is present in most of the professions and activities that human beings develop and of course, in medicine, one of the most notable and important disciplines since ancient times could not not present a weighty place.
Medical ethics or medical deontology, as it is also called, groups together a set of standards and principles that inspire and also guide the work of medical professionals.
Beyond the modalities applied by each professional individual, the principles that medical ethics proposes must yes or yes be observed and respected by the doctor.
All organizations doctors in the world have as a fundamental mission to promote and develop deontology and also postulate the principles in works of ethics that educate future professionals and practicing physicians when respect.
Of course, any breach of these will trigger a punishment.
Crucial principles: beneficence, autonomy, justice and non-maleficence
Among the most prominent principles are: charity (It will always involve acting for the benefit of others, putting aside prejudices and making the rights of others prevail. When the patient does not know the medicine, the doctor is obliged to act in the best way to ensure the good of it), autonomy (ability to impose rules and not fall under pressure from outside), Justice (treat everyone as they should without discrimination due to various conditions, that is, all patients should receive the same treatment) and no maleficence (It implies the abstention of those actions that may cause direct damage or harm in any way to others).
The principle of non-maleficence is considered the most relevant because it implies a commitment to something basic, which is not to incur direct or indirect harm to the patient.
When a doctor prescribes a treatment or surgical practice to a patient, she must assess the risks and the benefits, weigh them, and based on this decide whether or not to carry out the practice in question.
And with respect to the principle of autonomy that directly affects the patient and that allows him to be able to say whether or not to undergo a operation or treatment, the most emblematic example is that of informed consent, which consists of the patient giving his permission and acceptance in writing before the imminence of a medical practice.
That acceptance will mark his knowledge of the pros and cons of the practice to which he will submit.
Topics in Medical Ethics


